Your Second Brain: A Deep Dive into the Gut-Brain Axis and Mastering Your Mental Health Through Nutrition
Introduction – Why This Matters
For decades, we’ve separated mental health from physical health, treating the mind as an entity distinct from the body. Phrases like “it’s all in your head” have tragically minimized the biological underpinnings of psychological distress. What if the key to calming your anxiety, stabilizing your mood, and sharpening your focus wasn’t found solely on a therapist’s couch, but also on your dinner plate?
A seismic shift is occurring in psychiatry and neuroscience. We now understand that a continuous, bi-directional superhighway of communication exists between your brain and your gastrointestinal tract, primarily your gut microbiome—the trillions of bacteria, viruses, and fungi living within you. This is the gut-brain axis. Disruptions on this highway are now linked not just to digestive woes but robustly to conditions like Major Depressive Disorder, Generalized Anxiety, ADHD, and even neurodegenerative diseases.
In my experience working with clients struggling with persistent, low-grade anxiety and “brain fog,” dietary intervention focused on the gut has been a game-changer where traditional approaches had plateaued. What I’ve found is that while therapy addresses the software (thought patterns and behaviors), optimizing the gut-brain axis often fixes critical issues with the hardware, allowing therapeutic work to be far more effective.
This article will demystify the complex science of the gut-brain connection and provide you with a practical, step-by-step framework to harness its power for your mental well-being.
Key Takeaways
- Your gut microbiome produces neurotransmitters (like serotonin and GABA) and communicates with your brain via the vagus nerve, hormones, and immune messengers.
- Dysbiosis (an imbalanced gut) can directly contribute to inflammation, which is a key driver of depression and anxiety.
- You can measurably influence your microbiome and mental state through targeted dietary and lifestyle changes within weeks.
Background / Context
The concept of a gut-mind connection isn’t entirely new. Ancient healing systems like Ayurveda and Traditional Chinese Medicine have emphasized digestive health as the root of vitality for millennia. However, Western medicine remained skeptical until the advent of sophisticated genetic sequencing and neuroimaging tools in the last 15-20 years.
The pivotal realization was this: the human body is not a singular organism. We are a holobiont—a host in symbiotic partnership with a vast microbial ecosystem. These microbes collectively contain millions more genes than our human genome. They are not passive passengers; they are active participants in our physiology, digesting food, training our immune system, and, crucially, manufacturing an estimated 90% of the body’s serotonin (the “feel-good” neurotransmitter) and significant amounts of GABA (the primary calming neurotransmitter).
The old model of “brain as command center” has been replaced by a model of continuous, dynamic dialogue. Your brain sends signals to your gut (ever felt “butterflies” from nerves?), and your gut sends powerful signals back that profoundly alter your emotional and cognitive landscape.
Key Concepts Defined
- Gut-Brain Axis: The bidirectional communication network linking the central nervous system (brain and spinal cord) and the enteric nervous system (the complex system of neurons governing the gastrointestinal tract).
- Microbiome/Microbiota: The community of trillions of microorganisms (bacteria, archaea, fungi, viruses) living in a particular environment, notably the human gut. Often used interchangeably, though microbiota refers to the organisms themselves, and microbiome includes their genes and environment.
- Dysbiosis: An imbalance or maladaptation in the gut microbial community, often characterized by a loss of beneficial bacteria, an overgrowth of potentially harmful ones, and a reduction in overall diversity.
- Vagus Nerve: The longest cranial nerve, forming a primary physical communication channel between the gut and the brain. It transmits signals about gut state, inflammation, and nutrient availability.
- Psychobiotics: A class of probiotics (live beneficial bacteria) and prebiotics (food for those bacteria) that, when ingested, confer a mental health benefit.
- Leaky Gut (Intestinal Permeability): A condition where the lining of the small intestine becomes damaged, allowing undigested food particles, toxins, and bacteria to “leak” through the intestines and into the bloodstream, triggering systemic inflammation and immune responses.
How It Works: The Gut-Brain Communication Highway (Step-by-Step Breakdown)

The gut and brain communicate through multiple, overlapping pathways. Think of it as a sophisticated corporate network with different departments using various channels.
- The Neural Pathway (The Vagus Nerve Hotline): The vagus nerve is a direct phone line. Gut microbes produce neurotransmitters and metabolites (like short-chain fatty acids). These chemicals stimulate vagal nerve endings in the gut wall, sending signals up to the brainstem, which then relays them to higher brain regions involved in mood, fear, and cognition.
- The Immune Pathway (The Inflammation Alarm): Over 70% of the immune system resides in the gut. An imbalanced microbiome (dysbiosis) can trigger low-grade chronic inflammation. Pro-inflammatory cytokines (immune messenger molecules) can cross the blood-brain barrier, directly impacting brain function. This neuroinflammation is a cornerstone of depressive and anxious states.
- The Endocrine Pathway (The Hormonal Highway): The gut is a major endocrine organ. It produces gut hormones (like ghrelin and leptin) that influence appetite and stress. The microbiome also helps regulate the body’s primary stress response system, the HPA (Hypothalamic-Pituitary-Adrenal) axis. Dysbiosis can lead to a dysregulated, overactive stress response.
- The Microbial Metabolite Pathway (Chemical Messengers in the Bloodstream): Gut bacteria ferment dietary fiber to produce Short-Chain Fatty Acids (SCFAs) like butyrate, acetate, and propionate. SCFAs cross into the bloodstream, travel to the brain, and exert powerful anti-inflammatory effects, strengthen the blood-brain barrier, and may even promote the growth of new brain cells.
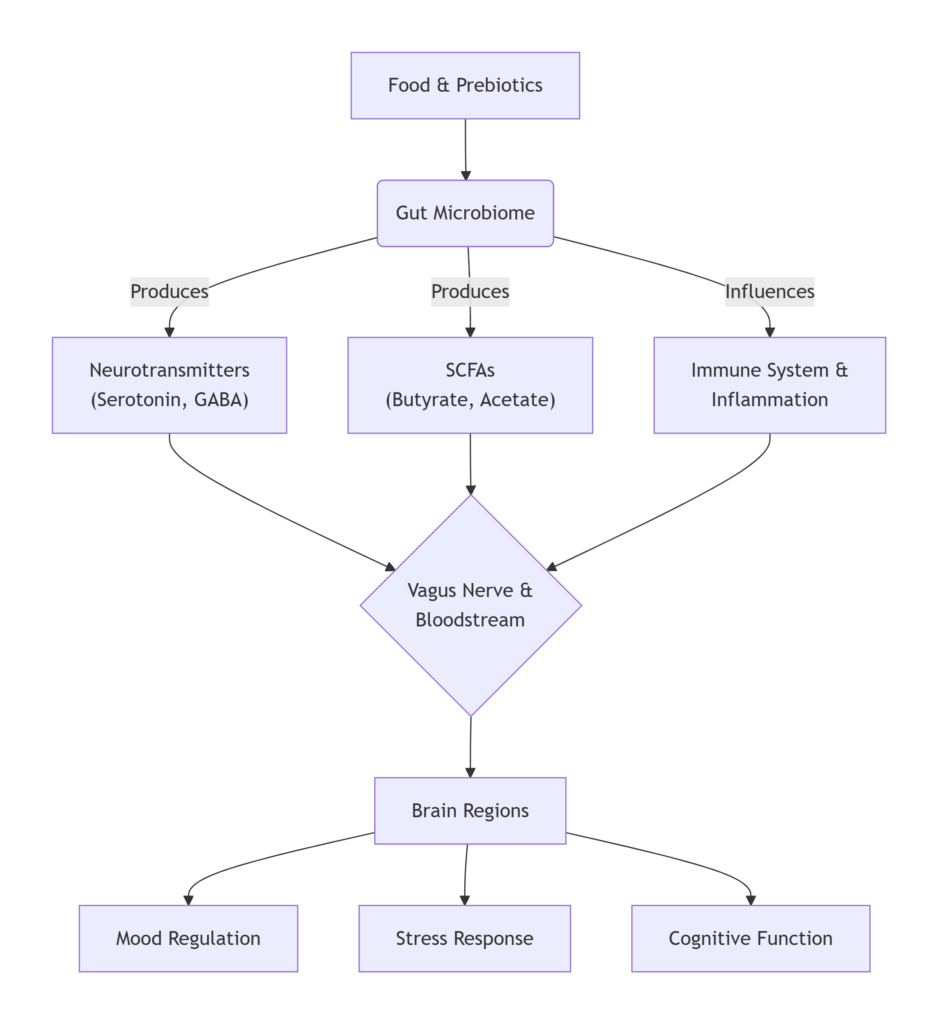
Simple Canva graphic illustrating the Gut-Brain Communication Pathways.
Why It’s Important
Ignoring the gut-brain axis means ignoring a fundamental pillar of mental health. The evidence is no longer anecdotal:
- A 2024 meta-analysis in Nature Mental Health concluded that individuals with Major Depressive Disorder consistently show altered gut microbiome compositions compared to healthy controls, with specific bacterial deficits linked to symptom severity.
- Research demonstrates that transferring gut bacteria from humans with depression into germ-free rats can induce depression-like behaviors in the animals.
- Clinical trials using specific probiotic strains (psychobiotics) are showing promising results in reducing symptoms of anxiety, depression, and perceived stress.
This isn’t about replacing therapy or medication. It’s about adopting a holistic, systems-based approach. For someone struggling with mental health, addressing the gut can reduce the inflammatory and biochemical burdens that make emotional regulation feel impossible, creating a more fertile ground for other interventions to succeed.
Sustainability in the Future: Personal and Planetary Health
Sustainable mental health care is proactive, accessible, and preventative. Focusing on diet and the microbiome empowers individuals with a degree of self-efficacy—you can actively participate in your healing daily. It’s also more sustainable for healthcare systems, potentially reducing reliance on more costly interventions downstream.
On a planetary level, a diet that nourishes a healthy microbiome—rich in diverse plant fibers—is also a diet that supports sustainable agriculture and lower carbon footprints compared to standard Western diets high in ultra-processed foods and red meat. Caring for our inner ecosystem aligns with caring for our outer one.
Common Misconceptions
- “Probiotic yogurt is all I need.” Most commercial yogurts contain limited strains in quantities that may not survive stomach acid or colonize the gut. A diverse, fiber-rich diet is far more important for cultivating a resilient microbiome.
- “This means my mental illness is my fault because of a bad diet.” Absolutely not. Mental illness is complex, with genetic, traumatic, social, and biological origins. Dysbiosis is one contributing biological factor, not a cause of blame. It’s a leverage point for healing.
- “I need expensive microbiome testing and custom supplements.” While testing can be informative, the foundational prescription is universal: eat a wide variety of whole, fermented, and fiber-rich foods. You don’t need a test to start eating more plants.
- “Improving my gut will cure my depression/anxiety overnight.” Changes in microbiome composition can begin within days, but translating to measurable mental health shifts often takes consistent effort over weeks or months, alongside other treatments.
Recent Developments (2024-2025)
- AI-Driven Personalization: Companies and research institutes are using machine learning to analyze microbiome data and predict individual responses to specific dietary components or psychobiotic strains, moving towards personalized nutrition for mental health.
- Postbiotic Therapeutics: The focus is shifting from live probiotics (bacteria) to postbiotics—the beneficial metabolic byproducts they produce (like specific SCFAs). These can be packaged as stable supplements with direct neuroactive effects.
- The “Gut-Brain Skin Axis”: New research is explicitly linking gut health, mental health, and inflammatory skin conditions like psoriasis and eczema, illustrating the systemic reach of the microbiome.
- Fecal Microbiota Transplants (FMT) & Mental Health: While primarily for C. diff infection, early, cautious trials are exploring FMT for treatment-resistant depression, with rigorous ethical and safety protocols.
Success Stories and Real-Life Examples
- The SMILES Trial (2017): This landmark study from Australia was one of the first randomized controlled trials to show that a modified Mediterranean diet (rich in whole grains, legumes, vegetables, and fish) could be an effective treatment strategy for major depression. Participants in the dietary intervention group saw significantly greater improvement in their depression scores than those in a social support control group.
- Personal Anecdote: A client of mine, “Sarah,” had managed generalized anxiety for years with therapy, which was helpful, but she still dealt with pervasive physical tension and “panic-like” gut feelings. After a 3-month protocol focused on eliminating gut irritants (like industrial seed oils and excess sugar), incorporating daily fermented foods (kefir, sauerkraut), and a massive increase in vegetable diversity, she reported: “The anxiety is still there, but it’s lost its physical edge. I can now use the breathing techniques from therapy because my gut isn’t screaming false alarms all day.” This decoupling of the gut’s distress signal was a turning point.
- Public Figure Advocacy: Numerous athletes and celebrities now speak openly about using gut health protocols to manage stress and mental performance, helping to destigmatize the link.
Conclusion and Key Takeaways
The mind is not an island. It is intimately woven into the fabric of the body, with the gut being its most vocal conversational partner. The science of the gut-brain axis provides a powerful, evidence-based rationale for why nourishing our bodies is fundamental to nurturing our minds.
This doesn’t demand perfection. It invites curiosity. Start by adding one extra vegetable to your meals, experiment with a fermented food, or notice how different foods make you feel—not just in your stomach, but in your mood and energy levels.
Your mental health journey is multifaceted. Continue your therapy, take prescribed medications in consultation with your doctor, foster social connections, and move your body. But also, feed your microbiome. It’s a crucial piece of the puzzle that has been missing for too long, offering a tangible path toward greater resilience and calm.
Final Key Takeaways:
- Your gut is a primary site for the production of key neurotransmitters.
- Chronic inflammation, often rooted in the gut, is a major contributor to depression and anxiety.
- The vagus nerve is the direct neural link between your gut state and your brain.
- You can positively influence this system through dietary diversity, focusing on plants and fermented foods.
- This approach is complementary, not alternative, to established mental health care.
FAQs: The Gut-Brain Axis
Q1: What’s the single most important dietary change I can make for my gut-brain health?
A: Dramatically increase the diversity and quantity of plant-based fibers. Aim for 30 different plants per week (herbs, spices, nuts, seeds, vegetables, legumes, grains). Fiber is the primary food for your beneficial gut bacteria.
Q2: Are probiotic supplements worth it?
A: They can be a helpful adjunct, especially specific psychobiotic strains like Lactobacillus helveticus and Bifidobacterium longum. However, they are not a substitute for a good diet. The effects are often strain-specific and temporary if not supported by dietary fiber.
Q3: Can gut health really help with ADHD?
A: Emerging research suggests a strong link. Inflammation can affect neurotransmitter function and brain energy metabolism. Many with ADHD report improvements in focus and emotional regulation with anti-inflammatory, gut-supportive diets, though it should complement, not replace, standard care.
Q4: How long does it take to see mental health changes from improving my diet?
A: Microbiome composition can start to shift in days. Some people report changes in energy and digestion within 1-2 weeks. More stable mood and cognitive effects may take 4-12 weeks of consistent practice.
Q5: What are the top inflammatory foods to avoid?
A: The primary culprits are: Ultra-processed foods (high in emulsifiers and additives that disrupt the gut lining), refined sugars and high-fructose corn syrup, industrial seed oils (high in omega-6, like soybean and corn oil), and for some, gluten and dairy (if sensitive).
Q6: Is there a link between gut health and autism spectrum disorder (ASD)?
A: Research is active in this area. Many individuals with ASD have significant gastrointestinal issues and distinct microbiome profiles. While not a cause, addressing gut health is often a key part of a comprehensive, integrative approach to improving quality of life and certain behaviors.
Q7: What are the best fermented foods for beginners?
A: Start with plain, unsweetened kefir (drink a small amount), sauerkraut (found in the refrigerated section, not canned), kimchi, or unsweetened kombucha. Begin with a teaspoon daily and work up to a few tablespoons to allow your system to adjust.
Q8: How does stress hurt my gut microbiome?
A: Chronic stress alters gut motility, increases intestinal permeability (“leaky gut”), and changes the gut environment, favoring less beneficial microbes. It’s a vicious cycle: stress hurts the gut, and a hurt gut amplifies the stress response.
Q9: Can antibiotics permanently damage my gut-brain axis?
A: While antibiotics can cause severe, long-term dysbiosis in some cases, the microbiome is generally resilient. Proactive replenishment with diverse fibers, fermented foods, and potentially probiotics after an antibiotic course is crucial for recovery.
Q10: What’s the connection between the gut and sleep?
A: A strong one. Your microbiome follows a circadian rhythm. Dysbiosis can disrupt melatonin production (much of which is made in the gut) and increase sleep-fragmenting inflammation. Improving gut health often leads to better sleep quality.
Q11: Should I try an elimination diet for anxiety?
A: Do not start a restrictive elimination diet without guidance, especially if you have a history of eating disorders. If you suspect food sensitivities, work with a registered dietitian or functional medicine doctor to do a structured, supervised elimination and reintroduction protocol.
Q12: Are prebiotics the same as fiber?
A: All prebiotics are fiber, but not all fibers are prebiotics. Prebiotics are specific types of soluble, fermentable fiber (like inulin, FOS, GOS) that selectively nourish beneficial bacteria. They are found in foods like garlic, onions, leeks, asparagus, and oats.
Q13: How does alcohol affect the gut-brain axis?
A: Alcohol is a gut disruptor. It can damage the gut lining, promote dysbiosis, and increase inflammation and endotoxin (bacterial toxin) translocation into the bloodstream—all negatively impacting the brain.
Q14: Is there a role for bone broth?
A: Bone broth contains collagen, gelatin, and amino acids like glycine and glutamine, which theoretically can support gut lining repair. While anecdotal reports are positive, robust clinical evidence is limited. It can be a nourishing part of a diet, butit isn’t a magic bullet.
Q15: Can children’s mental health be impacted by gut health?
A: Profoundly. Early-life microbiome development is critical for programming the immune system and brain. Mode of birth (vaginal vs. C-section), breastfeeding, early antibiotic use, and diet are major factors studied in relation to childhood anxiety, mood, and neurodevelopmental outcomes.
Q16: What about artificial sweeteners and the gut?
A: Studies on animals and some humans show that certain artificial sweeteners (like sucralose and saccharin) can alter the microbiome negatively and induce glucose intolerance. It’s wise to limit them.
Q17: Where can I learn more about science?
A: Follow the work of leading research organizations like the APC Microbiome Ireland and journals like Brain, Behavior, and Immunity and Gut Microbes. For a comprehensive guide on mental wellbeing foundations, see this excellent resource from The Daily Explainer: Mental Health: The Complete Guide to Psychological Wellbeing in the Modern World.
Q18: How does this relate to business performance and entrepreneurship?
A: Directly. Mental clarity, resilience under stress, emotional regulation, and sustained energy are the currencies of success. For entrepreneurs, managing the gut-brain axis can be a non-negotiable biohack for peak performance. Explore more on optimizing your work and life on World Class Blogs’ Remote Work & Productivity section.
Q19: I’m overwhelmed. What’s one simple first step?
A: Add, don’t subtract. This week, add one daily serving of a leafy green (spinach, kale, arugula) and one tablespoon of ground flaxseed to your breakfast or smoothie. That’s it.
Q20: Where can I find support and further resources on my health journey?
A: The Sherakat Network is here to help. Explore our curated Resources and insightful Blog for more guides. If you have specific questions, don’t hesitate to contact us.
About the Author
Sana Ullah Kakar is a certified integrative nutrition health coach and mental health advocate with a background in neuroscience. They have spent the last decade bridging the gap between cutting-edge nutritional psychiatry and practical, everyday wellness strategies. Their writing has appeared in various health publications, and they work one-on-one with clients to use diet and lifestyle as core tools for building mental resilience. They are passionate about empowering people with the knowledge that their bodies are a powerful ally in the quest for mental peace.
Free Resources
- “30 Plants in a Week” Tracking Sheet: A printable PDF to help you easily track and increase your plant diversity.
- Simple Gut-Supportive Meal Plan (3-Day Starter): Non-restrictive recipes focusing on easy-to-digest, fiber-rich meals.
- Fermented Foods at Home: A Beginner’s Guide to Sauerkraut: A step-by-step video tutorial.
- Vagus Nerve Stimulation Exercise Library: A PDF guide to 5 simple, daily exercises (like humming and diaphragmatic breathing) to tone your vagus nerve.
- For entrepreneurs looking to build holistic success, pair this knowledge with our foundational business guide: Start Online Business 2026: The Complete Guide.
Discussion
We’d love to hear from you!
Have you noticed a connection between what you eat and how you feel mentally? What’s your biggest challenge in implementing a gut-friendly diet? Share your experiences, questions, or success stories in the comments below. Let’s build a community of support and shared knowledge.
Further Reading on Sherakat Network:
- For insights on building supportive professional relationships that reduce stress, read The Alchemy of Alliance: A Guide to Successful Business Partnership.
- To understand different collaborative models that can impact your work-life balance, see our breakdown of Business Partnership Models.


